October 9, 2024
In its first two decades, Travis County’s hospital district has forged a unique path to bring care to the most vulnerable.
The public hospital model is probably familiar to most Americans, especially since it provides the setting for so many TV medical dramas. If you need emergency care or surgery, most major cities have a publicly owned-and-operated hospital to provide that care, regardless of your insurance or ability to pay. These hospitals, and the clinics that support them, are often called “safety net” healthcare systems, although in many cities they’re also sites for the most advanced care.
In most big Texas urban counties – including Harris, Dallas, Bexar, Tarrant, and El Paso – special districts were formed in the mid-20th century to take over public hospital systems that had formerly been owned and run by the counties themselves. Travis County was, and still is, just a little different.
 Brackenridge Hospital in 2007, before its name change to University Medical Center Brackenridge. The hospital was demolished in 2019 and is the site of the new 17-story University of Texas office tower known as Block 164.
Brackenridge Hospital in 2007, before its name change to University Medical Center Brackenridge. The hospital was demolished in 2019 and is the site of the new 17-story University of Texas office tower known as Block 164.
For most of the 20th century, Travis County’s safety-net hospital needs were met by Brackenridge Hospital, owned and run by the city of Austin. Travis County residents both inside and outside Austin’s city limits paid taxes to support “indigent healthcare,” but at two different rates and levels of service, with county residents not paying to support Brackenridge – only the clinics outside the city limits.
That began to change in 1995, when – after an accounting error left the city holding millions of dollars’ worth of unpaid medical debt – Austin contracted with the Daughters of Charity Health System, more commonly known as Seton, to provide hospital and specialty care to residents with low incomes. Together, the city and Seton covered the costs of hospital services, balancing funding with Seton’s mission to provide charity care.
At same time, Austin and Travis County jointly operated a network of low-cost primary care clinics known as the Community Health Centers (CHC). By the early 2000s, this network had grown to include more than a dozen sites and had been certified as a Federally Qualified Health Center (FQHC), which made them eligible for federal funding and assistance and increased the breadth of services available to patients.
Despite these efforts, local safety-net services remained fragmented, making it difficult for patients to know where to seek care, which in turn hindered better outcomes for more patients with low income. Improving health outcomes for patients with low income became much harder to achieve as Austin and Central Texas embarked on a 35-year run of population and economic growth unmatched by most U.S. metro areas. As low-income workers flowed into Travis County to build and service the new boomtown, housing costs spiked, and health care resources became ever more stretched.
So, thanks to the advocacy of many community leaders and health care providers, the Texas Legislature in 2003 passed a law allowing Travis County voters to create a hospital district if they so chose. That legislation also mandated that taxes going to health care be equalized across the city and county.
Laying the Foundation for Central Health
On May 15, 2004, Travis County voters approved by a 9.4-point margin the creation of a hospital district. As the city and county zeroed out their tax collections for health care, the new district levied property taxes to pay for care at Brackenridge, the Children’s Hospital of Austin (also operated by Seton), and the Austin Women’s Hospital (operated by the UT Medical Branch at Galveston).
These were all located at the Downtown hospital campus at 15th Street and IH-35. The district also took ownership of 14 city and county-owned health clinics and the longstanding health coverage program for low-income residents known as the Medical Assistance Program, more commonly known as MAP (today, MAP stands for the Medical Access Program).
Early Growth and Developments
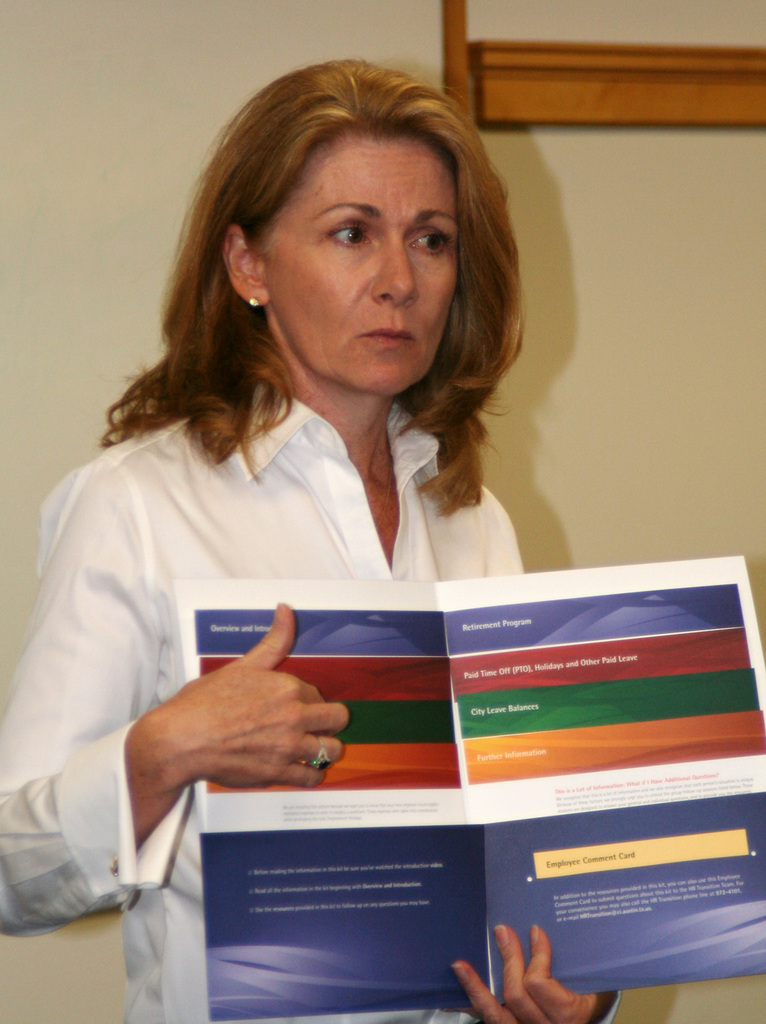
In 2005, Patricia A. Young Brown, who had been the director of the city/county clinic system, became the first President & CEO of what was now called the Travis County Healthcare District, hired by its nine-member all-volunteer Board of Managers. Under Young Brown’s leadership, and with her extensive experience in public finance, the organization began to craft a vision and strategic goals and drafted fiscally sound budgets to facilitate those plans.

Patricia Young Brown, then Senator Kirk Watson, Central Health Board Chair Rosie Mendoza, and Austin Mayor Lee Leffingwell cut the ribbon for the grand opening of the North Central Health Center on Braker Lane.
First up were numerous, significant, and long-needed investments in health care infrastructure. These included $250,000 for the expansion of the Shivers Cancer Center in East Austin and $1.6 million to rebuild Brackenridge’s intensive care unit. Mental health services, long hampered by a lack of dedicated funding, were addressed by a psychiatric services stakeholder committee which helped formulate an interim plan to expand access to mental health care. The Travis County Healthcare District was off to a running start.
In 2006, the newly expanded Brackenridge Hospital Emergency Department was unveiled. A year later, the district invested more than $1 million to bring trauma services at Brackenridge up to Level I standards (the highest level, which formerly required patients’ transfer to San Antonio or Bell County) and delivered the first fruits of its mental health plans, nearly $2 million to increase capacity at Seton’s Shoal Creek Hospital.
By 2008, the district was able to expand its reach and build the first new community health center in several decades – the state-of-the-art North Central Health Center on Braker Lane, in a fast growing and high-need area of the region – while providing $3.5 million for further expansions at the newly renamed University Medical Center Brackenridge (UMCB), which saw its trauma capacity double and psychiatric emergency care expanded. That same year, the district brought some long-needed streamlining to MAP by launching a mail-in recertification system, allowing members to re-enroll without the need for in-person appointments.
In 2009, the Travis County Healthcare District adopted the name it still has today, Central Health. That year Central Health created an affiliated nonprofit health center system, now known as CommUnityCare Health Centers, to operate Central Health’s clinic system and provide it with patient-centered governance, as is required of FQHCs. Up until this point, the district had paid the city to keep running its clinics to avoid disruptions for both patients and employees; those personnel transitioned to become employees of Central Health, which CommUnityCare staffers still are.
Expansion and Partnerships
The 2010s saw Central Health scaling up its efforts to expand access and improve the quality of care for patients with low income. Taking a square look at data showing Texas’ corps of primary care providers shrinking even as its population continued to boom, Central Health took the lead in an ambitious project, backed by numerous community leaders including Austin’s former and future Mayor Kirk Watson (at the time, its state senator), to found a new medical school at The University of Texas at Austin.

Proposition 1 supporters, including now Travis County Judge Andy Brown, Austin Mayor Kirk Watson, State Senator Eddie Rodriguez, State Representative Elliott Naishtat, Central Health Board Member Clark Heidrick, and Judge Guy Herman, celebrate the election night win in 2012.
The UT System operated medical schools elsewhere in the state, including ones affiliated with safety-net hospital systems in Dallas, San Antonio, and Houston, but the system’s flagship campus did not have a medical school – that was the consolation prize for Galveston when it lost the statewide referendum to host the main campus, back in 1881. In 2012 Central Health proposed raising its tax rate by five cents – which required voter approval – to fund health care expansion in Travis County, including earmarking funds for a medical school “consistent with the purposes of Central Health.”
In November 2012, voters agreed with the prognosis and – again by a 9.4-point margin –approved raising their own taxes to fund Central Health’s ongoing partnership with UT-Austin and the UT System. Since accepting its first students in 2015, the Dell Medical School has trained more than 1,000 new physicians, more than 500 of whom are focused on primary care.
Nearly half of these new doctors practice in Central Texas after they graduate. Dell Med and its teaching hospital, the Dell Seton Medical Center, are currently training 465 medical residents, including graduates of Dell Med and other medical schools, almost all of whom are working in clinics that serve low-income patients. Those residents have provided more than 1.2 million hours of care.
New Facilities and Services
In the last decade, Central Health continued expanding its role as a partner, planner, payor and provider in Travis County’s health care landscape. In 2016, the Southeast Health & Wellness Center opened, hosting a CommUnityCare clinic alongside numerous other services- from cooking classes to yoga to parenting, in the former Veteran’s Administration clinic on Montopolis. The following year, in time for Dell Med’s first classes of doctors-in-training, safety net hospital services moved from the aging Brackenridge campus to the new Dell Seton Medical Center across the street, freeing up the 13-acre Central Health Downtown Campus for reuse and redevelopment.
During that same era, Central Health experienced its first major change in leadership with Trish Young Brown’s retirement in 2016 and the hiring of Mike Geeslin as her successor the following year. Under Geeslin’s guidance, Central Health expanded its community outreach efforts to build relationships that would guide the launch of new services, improve existing ones, and shape new facilities, including the Central Health Hornsby Bend and Del Valle Health & Wellness Centers in eastern Travis County. Hornsby Bend opened in October 2023, and Del Valle is set to open in December 2024.

Board of Managers Member Cynthia Valadez, Travis County Commissioner Margaret Gomez, AISD Tgrustee and community advocate Ofelia Zapata, City Council Member Pio Renteria, and former City Council Member and current County Attorney Delia Garza cut the ribbon for the grand opening of the Southeast Health & Wellness Center in 2016.

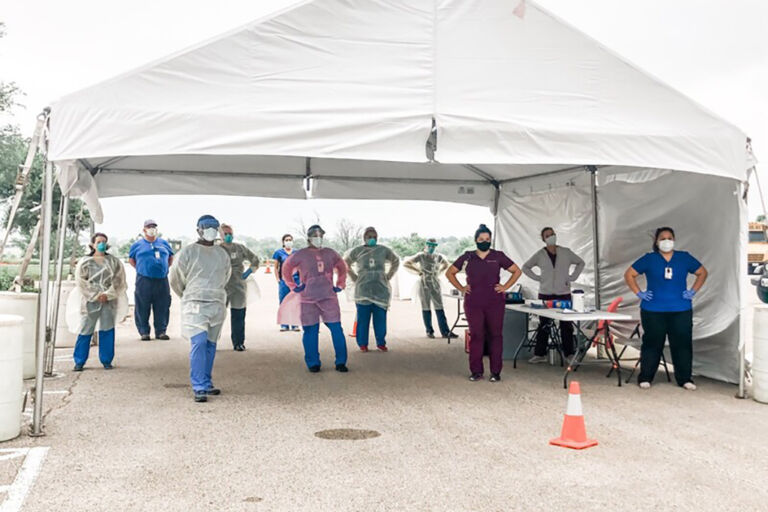
Central Health and CommUnityCare staff operated many drive-through COVID testing and vaccine sites for much of 2020 and 2021.
When the COVID-19 pandemic came to Central Texas in the spring of 2020, Central Health took the lead to protect less connected, low-income residents in rural and exurban communities in Travis County. With Central Health’s CommUnityCare at the forefront of its pandemic response efforts, the district partnered with Austin Public Health, and Travis County to provide essential care and, in 2021, access to the vaccines that turned the tide of the outbreak.
Growth, change, and a new role
The COVID-19 experience highlighted how fragmented and insufficient Travis County’s safety-net healthcare system was to meet the health needs of a growing urban area. Central Health responded with a comprehensive strategic planning initiative that led to its 2022 Healthcare Equity Plan, a comprehensive blueprint for addressing health care disparities in Travis County as well as a long-term roadmap for delivering equitable care to all residents.
 The Central Health Equity Policy Council after a successful campaign to have vaping banned in shared indoor spaces.
The Central Health Equity Policy Council after a successful campaign to have vaping banned in shared indoor spaces.
Implementation of the Healthcare Equity Plan will be ongoing through at least the end of fiscal year 2030, and Central Health expects to invest more than $800 million to launch and staff up the services that would close the gaps revealed by the plan’s needs assessment. The district has managed its reserve funds to make sure that money is available when it’s needed.
After seven years at the helm, Geeslin left Central Health at the end of 2023, and Dr. Patrick Lee became Central Health’s new president and CEO in February 2024. A practicing physician, Dr. Lee brought a different background and philosophy to the role, one that meshes well with Central Health’s growth as a direct practitioner of medicine. By the end of 2024, Central Health launched nearly 20 new specialty care and diagnostic lines of service, closing gaps that had existed since the healthcare district was founded and making access to advanced care a reality for MAP members.
Looking ahead to its third decade, Central Health continues to repair holes in the health care safety net and deliver more integrated, comprehensive, seamless care that leads to better outcomes for the people it serves. From caring for people experiencing homelessness, to providing Austin’s music community with access to health coverage, to equity-driven care for the LGBTQIA+ community, Central Health continues to deliver on the promise it’s made to the people of Travis County for more than two decades: By caring for those who need it most, Central Health improves the health of the entire community.